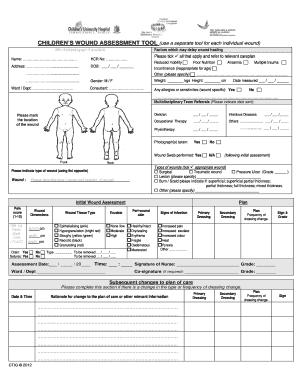
Stratis Health Wound Record Weekly Wound Assessment 2011-2025 free printable template
Show details
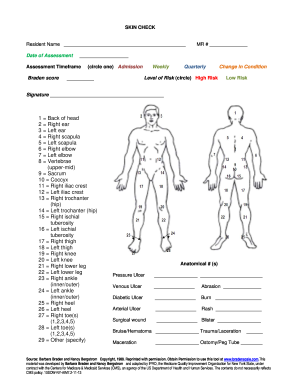
Wound Record Weekly Wound Assessment (Use a separate sheet for each wound site) Patient Information: Name Incontinence/moisture Altered sensory perception Risk Factors Altered nutritional status Activity
pdfFiller is not affiliated with any government organization
Get, Create, Make and Sign printable wound assessment form
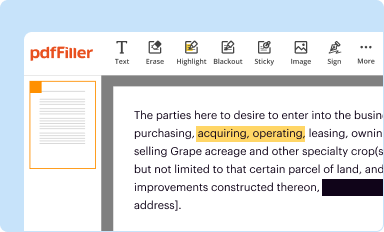
Edit your printable wound care documentation forms form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
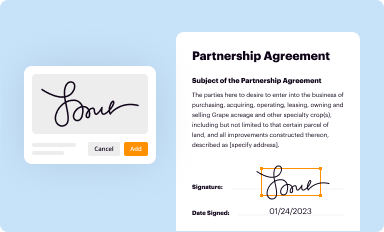
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
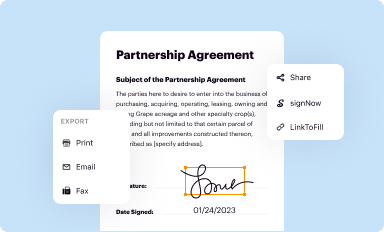
Share your form instantly
Email, fax, or share your wound care documentation template form via URL. You can also download, print, or export forms to your preferred cloud storage service.
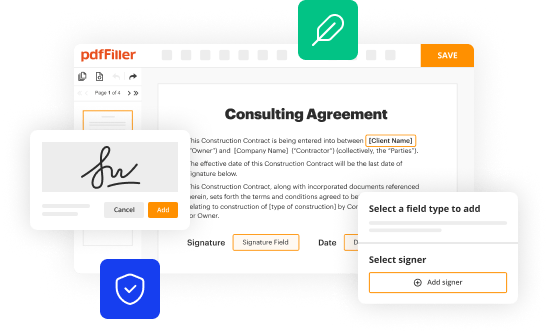
Editing wound measurement ruler printable pdf online
In order to make advantage of the professional PDF editor, follow these steps:
1
Check your account. If you don't have a profile yet, click Start Free Trial and sign up for one.
2
Prepare a file. Use the Add New button. Then upload your file to the system from your device, importing it from internal mail, the cloud, or by adding its URL.
3
Edit wound measurement tool printable form. Add and replace text, insert new objects, rearrange pages, add watermarks and page numbers, and more. Click Done when you are finished editing and go to the Documents tab to merge, split, lock or unlock the file.
4
Get your file. Select the name of your file in the docs list and choose your preferred exporting method. You can download it as a PDF, save it in another format, send it by email, or transfer it to the cloud.
The use of pdfFiller makes dealing with documents straightforward.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
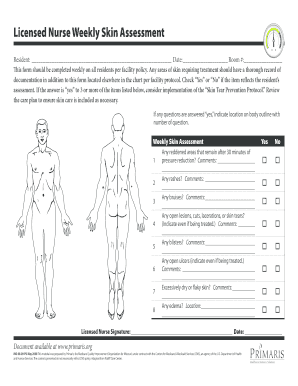
How to fill out weekly skin assessment form
How to fill out Stratis Health Wound Record Weekly Wound Assessment
01
Begin by obtaining the Stratis Health Wound Record form.
02
Fill in patient identification details including name, ID, and date.
03
Document the date of the assessment and the name of the person conducting it.
04
Assess the wound and note its dimensions (length, width, depth).
05
Describe the wound's appearance, including color, tissue type, and the presence of exudate.
06
Measure and record the wound's drainage levels and odor, if any.
07
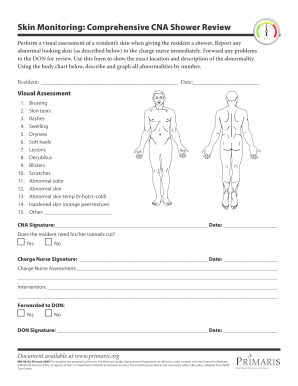
Evaluate the surrounding skin for signs of infection, redness, or other abnormalities.
08
Document any changes in the wound's condition since the last assessment.
09
Record the treatment interventions used during the week.
10
Conclude with recommendations for further treatment or adjustments to care.
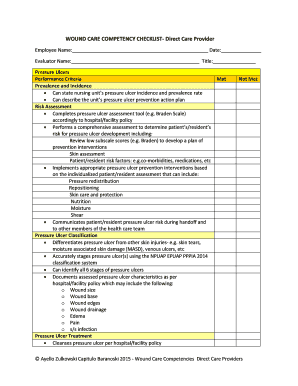
Who needs Stratis Health Wound Record Weekly Wound Assessment?
01
Patients with chronic wounds requiring regular assessment and documentation.
02
Healthcare professionals involved in wound care management.
03
Nurses and caregivers responsible for monitoring wound healing progress.
Fill
wound care template
: Try Risk Free
Our user reviews speak for themselves
Read more or give pdfFiller a try to experience the benefits for yourself
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I get Stratis Health Wound Record Weekly Wound Assessment?
It's simple with pdfFiller, a full online document management tool. Access our huge online form collection (over 25M fillable forms are accessible) and find the Stratis Health Wound Record Weekly Wound Assessment in seconds. Open it immediately and begin modifying it with powerful editing options.
How do I edit Stratis Health Wound Record Weekly Wound Assessment online?
With pdfFiller, the editing process is straightforward. Open your Stratis Health Wound Record Weekly Wound Assessment in the editor, which is highly intuitive and easy to use. There, you’ll be able to blackout, redact, type, and erase text, add images, draw arrows and lines, place sticky notes and text boxes, and much more.
How can I fill out Stratis Health Wound Record Weekly Wound Assessment on an iOS device?
pdfFiller has an iOS app that lets you fill out documents on your phone. A subscription to the service means you can make an account or log in to one you already have. As soon as the registration process is done, upload your Stratis Health Wound Record Weekly Wound Assessment. You can now use pdfFiller's more advanced features, like adding fillable fields and eSigning documents, as well as accessing them from any device, no matter where you are in the world.
What is Stratis Health Wound Record Weekly Wound Assessment?
Stratis Health Wound Record Weekly Wound Assessment is a systematic documentation tool used to evaluate and track the healing progress of wounds on a weekly basis, helping healthcare providers manage patient care effectively.
Who is required to file Stratis Health Wound Record Weekly Wound Assessment?
Healthcare providers, including nurses and physicians involved in wound care management, are required to file the Stratis Health Wound Record Weekly Wound Assessment for patients with wounds needing ongoing evaluation.
How to fill out Stratis Health Wound Record Weekly Wound Assessment?
To fill out the Stratis Health Wound Record Weekly Wound Assessment, healthcare providers should gather relevant patient information, assess the wound condition, document specific observations, and update any treatment plans based on the findings.
What is the purpose of Stratis Health Wound Record Weekly Wound Assessment?
The purpose of the Stratis Health Wound Record Weekly Wound Assessment is to monitor the healing process of wounds, identify potential complications, and ensure appropriate treatment interventions are applied in a timely manner.
What information must be reported on Stratis Health Wound Record Weekly Wound Assessment?
The information that must be reported includes patient identification, date of assessment, wound assessment findings (size, depth, appearance, exudate), pain levels, treatment provided, and any changes in the wound condition or patient response.
Fill out your Stratis Health Wound Record Weekly Wound Assessment online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Stratis Health Wound Record Weekly Wound Assessment is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.